What to Know About Restless Leg Syndrome (RLS) and Pregnancy
Dealing with pregnancy changes is stressful enough, but if you experience restless leg syndrome, the stress of the days can seep into the nights. RLS is a common condition of the nervous system that causes an overwhelming urge to move your legs, often disrupting your ability to get a good night's sleep. To help you better understand what to expect, we'll review some key information regarding restless leg syndrome and pregnancy.
What is Restless Leg Syndrome?
Restless leg syndrome, also known as Willis-Ekbom disease, is a neurological disorder characterized by an irresistible urge to move the legs, often accompanied by uncomfortable sensations such as tingling, itching, burning, or aching. While RLS can happen to anyone, women tend to experience it twice as often as men.
Is Restless Leg Syndrome Harmful to Your Baby?
Developing restless leg syndrome in pregnancy doesn't have any direct harm to your baby, but it can make it difficult to get a good night's sleep. There has also been a link between RLS and longer labor times or an increased risk of a cesarean section. Discussing your birth plan and preferences with your doctor or midwife can help you prepare for these scenarios if they occur.
Symptoms of Restless Leg Syndrome
The primary symptom of RLS is an overwhelming urge to move your legs or a generally unpleasant feeling in your lower limbs. Symptoms can sometimes vary in severity and become increasingly painful as they persist. They may be present one night and disappear the next, or they may be consistent throughout your pregnancy.
If you experience symptoms during pregnancy, you'll likely feel one or more of the following sensations in your feet and legs:
- Tingling feeling in the legs
- Feelings of restlessness
- Leg cramps
- Itching or burning
- A feeling like something is creeping or crawling on your legs
- Static or "fizziness" in the veins
These feelings tend to occur mostly below the knee but can also affect other areas of the body. Some women also experience symptoms in their thighs and arms. Typically, symptoms get worse during periods of rest, like when you're trying to get to sleep or when you've been sitting down for long periods of time. Worsening symptoms of RLS can result in sleep deprivation that affects your quality of life, mental health, and—since drowsiness can increase the risk of accidents—physical safety.
What to Know About Pregnancy and RLS
About 1 in 5 pregnant women will experience RSL in the third trimester of pregnancy. Experts aren't entirely sure why this happens, but many believe that hormonal changes contribute to its onset. Luckily, symptoms usually disappear after you've delivered your baby.
Iron deficiency anemia may also increase your likelihood of getting RLS. Since this deficiency is quite common during pregnancy, it's one theory of why so many expecting mothers experience RLS. Your doctor will check your iron levels during prenatal appointments and may recommend taking iron supplements if your levels are low. However, don't take any supplements or medications during pregnancy without first getting clearance from your doctor.
Certain medications used may also make symptoms worse. These include:
- Antihistamines
- Antidepressants
- Antipsychotics
- Lithium
- Antiepileptic drugs
- Beta-blockers
- Dopamine blocking agents
If you take any of these medications and experience mild to severe symptoms of RLS, talk to your doctor. However, do not stop taking any medications without discussing it with your doctor, as doing so can cause more harm than RLS.
What Else Causes Restless Leg Syndrome?
As mentioned, there is no known exact cause of restless limb syndrome. RLS outside of pregnancy may also occur from iron deficiency or even kidney failure. Some neurologists also believe it occurs due to how the brain and body process dopamine, the neurotransmitter responsible for pleasure, motivation, learning, and muscle movement.
Are Restless Leg Syndrome and Periodic Limb Movement Disorder the Same?
Periodic limb movement of sleep (PLMS) is a sleep disorder that causes repetitive jerking or twitching of the legs but can also affect the arms. This usually happens every 5 to 90 seconds, sometimes lasting through the night. PLMS is not the same as RLS. With restless leg syndrome, individuals voluntarily move their legs after feeling uncomfortable sensations to get relief. With periodic limb movement of sleep, movements occur subconsciously, often without "waking" those affected. However, more than 80% of people with RLS also experience PLMS. If you experience RLS during pregnancy, your doctor may also check for PLMS to help you find an appropriate treatment.
Treating RLS in Pregnancy
Unfortunately, the medications used to treat symptoms of RLS are not recommended during pregnancy and breastfeeding, so you'll need to take a more natural route. Still, your doctor may recommend a few diagnostic tests to rule out more dangerous conditions. This is done to rule out a potentially serious condition called deep vein thrombosis (DVT), which can present similar symptoms.
Fortunately, if you experience RLS in the last few months of pregnancy, it will most likely go away after giving birth. If issues persist, talk to your doctor about medications to improve symptoms.
Tips to Help with Restless Leg Syndrome During Pregnancy
Luckily, many healthy lifestyle changes can benefit restless leg syndrome and pregnancy. Some tips to help with bothersome symptoms include:
- Deep Relaxation Techniques — Deep relaxation techniques like meditation or progressive muscle relaxation can help alleviate symptoms by reducing stress, which can exacerbate RLS.
- Prenatal Yoga — Prenatal yoga can improve circulation and flexibility, potentially reducing discomfort associated with RLS and promoting better sleep.
- Regular Exercise and Movement — Regular exercise and movement, such as walking or gentle stretching, can help reduce RLS symptoms by improving blood flow and releasing endorphins that may alleviate discomfort.
- Regular Massage — Getting a massage, particularly of the legs and feet, can provide relief from RLS symptoms by loosening tight muscles and helping you feel more at ease.
- Warm Baths — A warm bath near bedtime can help soothe RLS symptoms by relaxing muscles and calming the nervous system, facilitating better sleep. Just make sure the water is not too hot so it's safe for your baby. A heating pad applied to the legs at night can also help.
- Cold Foot Baths — Cold foot baths or applying cold packs to the legs can temporarily alleviate RLS symptoms by numbing sensations and reducing inflammation.
- Extra Potassium — Increasing potassium intake through foods like bananas, sweet potatoes, and spinach, or supplements under medical supervision, may help alleviate RLS symptoms, as potassium plays a role in muscle function and nerve transmission.
- Prenatal Vitamins — Taking prenatal vitamins, especially those containing iron, folate, and magnesium, can help alleviate symptoms by addressing potential nutrient deficiencies that may contribute to restless legs during pregnancy.
You should also try to avoid caffeine in any amount if you experience RLS. Caffeine can worsen symptoms and make it harder to fall asleep, so switching to herbal teas and decaf coffee is recommended. Also, try to only get in bed once you're tired and ready to fall asleep. The longer you lie in bed, the more likely symptoms will develop. If you're unable to sleep or experiencing insomnia from RLS, getting out of bed can help.
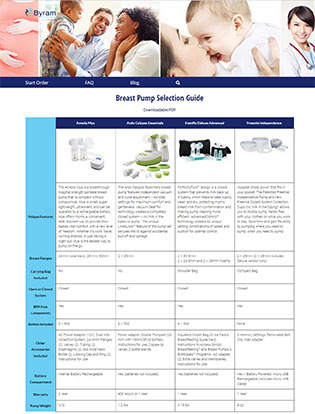
A lack of sleep during pregnancy can be extremely frustrating, especially when you know that the not-so-silent nights are right around the corner. While lifestyle changes can help you manage pain or feelings of discomfort, working with your doctor is the best way to ensure you have a treatment plan that's right for you. To help you support a healthy breastfeeding journey after delivery, Byram Healthcare has plenty of resources, experts, and products available. We also have a large selection of free breast pumps through insurance available to new and expecting mothers to help supplement their nursing sessions. This is a great way to share feedings with your partner or other caregivers, giving you time to nap, rest, or just want to sit on the couch in peace. To learn more, visit our breast pump product guide and start your order today.