Everything You Need to Know About Breastfeeding Jaundice
Breastfeeding is the best way to provide your child with essential nutrients and minerals for development. However, babies who breastfeed tend to have a higher risk of developing jaundice than those who are fed formula. Usually, this is nothing to be worried about and babies with breastfeeding jaundice recover quickly. To make sure that you take the proper care and seek medical treatment swiftly, we’ll cover everything you need to know about breastfeeding jaundice.
What is Breastfeeding Jaundice?
Bilirubin is a byproduct that occurs as red blood cells are broken down in the liver. This is a natural process that occurs in everyone, from newborns to the elderly. Sometimes, bilirubin can become elevated, which results in jaundice. This can happen for a number of reasons, but in regard to newborns, it’s usually harmless. The Centers for Disease Control and Prevention states that bilirubin could be elevated in newborns due to any of the following reasons:
- Newborns have an increased rate of bilirubin production due to short lifespan of red blood cells and high red blood cell concentration
- Newborns have immature liver function, which results in a slower metabolism of bilirubin
- Newborns may have a delay in the passage of meconium, which results in bilirubin reabsorption through the intestines
Breastfeeding jaundice usually occurs during the beginning of a newborn’s life, while they’re getting used to breast milk. It’s also referred to as suboptimal intake jaundice or physiologic jaundice, as it’s usually directly related to inadequate milk intake while new moms work to maximize latching and create regular feeding schedules. This is an extremely common occurrence and happens in about 60% of full-term babies and 80% of preterm babies within their first week of life. Infant jaundice is in no way the mother’s fault. You may also hear it referred to as infant jaundice.
The Difference Between Breastfeeding Jaundice and Breast Milk Jaundice
Breastfeeding jaundice is common and has a clear, underlying cause. It’s associated with your baby’s young age and developing systems in addition to their lack of milk intake while establishing breastfeeding. It can be easily treated and reversed once milk intake increases, and your newborn’s organs continue to develop.
Breast milk jaundice refers to a type of jaundice that continues to last several weeks after birth. It can occur in healthy babies and the cause is less understood than breastfeeding jaundice. Doctors believe that it may have something to do with the inability to break down and process bilirubin, as it tends to have a genetic association. There are still plenty of ways to treat breast milk jaundice and there’s no reason to expect lasting complications or injuries. However, it’s important to work with your pediatrician to continue to monitor bilirubin levels and development. Unlike breastfeeding jaundice, breast milk jaundice is rare and affects fewer than 3% of infants.
Symptoms of Breastfeeding Jaundice
The most recognizable symptom of jaundice is yellowing of the baby’s skin and eyes. In the case of breastfeeding jaundice, this usually occurs between the second and fourth day after birth but can be easily missed as the color may not be very noticeable. To check for signs of infant jaundice, gently press on your baby’s nose or forehead. If the lingering skin looks yellow, it’s an indication of mild jaundice. While this can be alarming for new parents, take a few deep breaths and try not to worry. Breastfeeding jaundice is common and, in most cases, it’s not a sign of more serious underlying medical conditions. If the skin appears lighter but with no yellow tint, your baby does not have jaundice.
Signs or symptoms of severe breastfeeding jaundice should prompt immediate medical attention. An extremely high concentration of bilirubin can affect brain development, so don’t wait if you notice any of the following:
- Increased yellowing of the skin
- Yellowing of the skin on your baby’s arms, legs, or abdomen
- Yellowing of the whites of your baby’s eyes
- Lack of weight gain or infrequent feedings
- Listlessness or signs of sickness
- Difficulty waking up
- High-pitched crying
These can indicate that the jaundice is worsening, which may point to an underlying cause that needs to be addressed. See your pediatrician to undergo diagnostic testing and begin treatment.
Breastfeeding Jaundice Causes and Risk Factors
Breastfeeding jaundice is directly caused by elevated bilirubin levels. Bilirubin can accumulate in your newborn’s system if their liver isn’t efficient enough to remove all of the bilirubin from their bloodstream. This is nothing to worry about, as it’s a common condition that occurs in babies born before 38 weeks and breast-fed babies. As their liver continues to develop, breastfeeding jaundice should pass. Again, this is often referred to in the medical community as physiologic jaundice.
Infant jaundice can also occur due to an underlying disorder. In this case, it may develop immediately following birth or after a few weeks of life. Some of the potential causes of this type of infant jaundice include:
- Internal bleeding
- Viral or bacterial infection
- Infection of the blood
- Incompatibility between the mother’s blood and the baby’s blood
- Liver malfunction
- Biliary atresia
- Enzyme deficiencies
- Red blood cell abnormalities
There are also several risk factors that may increase your baby’s chance of developing infant jaundice. While many of these are not preventable, it’s important to be aware of them so you can watch for any signs or symptoms that may indicate jaundice.
- Premature Birth – if your baby was born before 38 weeks, they will have an increased risk of developing infant jaundice since their liver is underdeveloped.
- Bruising During Birth – if your baby was severely bruised during the delivery process, they may be at a higher risk for infant jaundice as bruising results in the breakdown of red blood cells.
- Blood Type – when moms and their babies have different blood types, it increases the risk of jaundice as shared antibodies that don’t match can cause an initial breakdown of red blood cells.
- Breast-Feeding – babies who breastfeed but struggle to latch may show signs of jaundice, as they don’t initially receive enough nutrition. Working with a lactation consultant can help you mitigate these risks as breastfeeding is still the preferred choice of nutrition for newborns.
- Race – babies of East Asian descent tend to have higher levels of infant jaundice than their counterparts.
Diagnosing and Treating Breastfeeding Jaundice
Babies that were born between 35 weeks of gestation and full term rarely need treatment for breastfeeding or infant jaundice. As their organs continue to develop, their liver will become more capable of filtering out the bilirubin and jaundice will dissipate on its own. However, it’s important that you see your pediatrician at the first sign of jaundice for further care. They will be able to help you understand signs or symptoms to look for that may indicate an underlying condition or dangerous complications that, although rare, can occur with infant jaundice.
Since infant jaundice tends to occur in the first few days following birth, your hospital or birthing center will perform an examination to check for signs of jaundice prior to discharging you. They’ll also perform continual checks during your stay. The American Academy of Pediatrics recommends checking newborns for jaundice every eight to 12 hours while in the hospital and again during every routine checkup with their pediatrician.
Blood tests can be done to check the amount of bilirubin in your baby’s system. This will allow your pediatrician to provide the correct course of treatment. In many cases, improving nutritional intake is enough to reverse signs of jaundice and support a healthy development. However, if this isn’t enough, your pediatrician may recommend a few different options. Treatment for infant jaundice can include:
- Phototherapy – this involves treating jaundice with special lamps that can affect the shape and structure of bilirubin. The transformation allows excess bilirubin to be excreted through urine and stool.
- Intravenous Immunoglobulin – if jaundice is related to differences in blood type, IVIg may be recommended to reduce the antibodies that are causing the rapid deterioration of red blood cells.
- Exchange Transfusion – in rare instances, jaundice that doesn’t respond to other treatments may be treated using a blood transfusion. This is often performed in an intensive care unit to ensure the safest environment and ongoing monitoring.
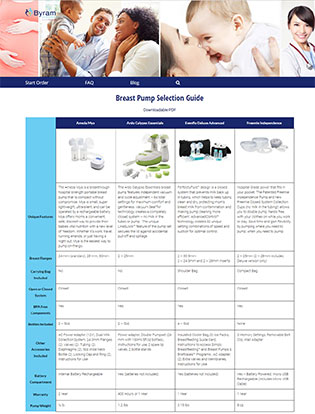
Breast pumping can help you supplement your nursing sessions and reduce the risk of infant jaundice. To help ensure that your baby is getting the nutrients they need for a healthy development, Byram Healthcare offers a wide selection of insurance covered breast pumps to new and expecting moms. Browse our breast pump comparison chart and get started with our easy, three-step ordering process today.