What to Expect if Your Baby is in the NICU
Welcoming a newborn into the world is meant to be an overwhelmingly positive experience, but if your baby is born prematurely or with health complications, it can be hard to stay optimistic. In such cases, your baby may require additional medical attention in a Neonatal Intensive Care Unit (NICU). The NICU is a unique and highly specialized environment, but it can also be a scary place. To help, here’s information on what to expect if your baby is in the NICU.
What is the NICU?
The Neonatal Intensive Care Unit (NICU) is a specialized unit in a hospital where critically ill or premature newborns receive intensive medical care. Infants who require care in the NICU are usually those who are born before 37 weeks of gestation or those who have serious health problems that require specialized medical attention.
In the NICU, newborns are monitored closely, receive specialized treatments, and may require assistance with breathing, feeding, and other functions. The goal of the NICU is to provide the highest level of care to help fragile newborns grow and develop, and eventually go home with their families. The American Academy of Pediatrics has four distinct categories based on the level of care the facility can provide to newborns. These include:
Level I (Well Newborn Nursery)
Level I units are referred to as the well newborn (or well baby) nursery and provide basic care for healthy newborns. They may provide some special care for infants born prematurely or with minor health issues. Level I units are typically found in hospitals with maternity units and don’t have advanced medical equipment or specialized medical staff.
Level II (Special Care Nursery)
Level II NICUs provide care for moderately ill newborns who require more specialized monitoring and treatment. They may have equipment for continuous monitoring of vital signs, as well as specialized equipment for feeding and respiratory support. Level II units typically have pediatricians, neonatologists, and specialized nurses on staff. They also have everything available to care for newborns in Level I units.
Level III Neonatal Intensive Care Unit
Level III NICUs provide comprehensive care for critically ill newborns who require advanced medical interventions, such as mechanical ventilation, surgery, and specialized medications. They have the highest level of medical and nursing expertise, with neonatologists, pediatric surgeons, and other specialists available 24/7. Level III NICUs are equipped with the most advanced medical equipment and technology, including advanced respiratory support, extracorporeal membrane oxygenation (ECMO) machines, and a range of diagnostic and therapeutic tools. They also have everything available to care for newborns in Level I and Level II units.
Level IV (Regional NICU)
Level IV NICUs are regional centers of excellence for neonatal care, providing the most advanced and specialized care for the most fragile newborns. They have all the capabilities of Level III NICUs (and Level I and Level II units), as well as added resources and expertise to provide care for the most complex medical conditions, including congenital abnormalities, genetic disorders, and multiple births. Level IV NICUs typically have research programs, as well as educational and training programs for healthcare professionals.
Who Works in the NICU?
The medical staff in the NICU includes neonatologists, pediatric nurses, respiratory therapists, and other healthcare professionals who specialize in caring for sick or premature newborns.
Specialist Nurses
Neonatal nurse practitioners (NNPs) are nurses who specialize in supplying critical care to newborns in the NICU. They work alongside doctors and neonatologists to provide treatment for a variety of ailments. Neonatal nurse practitioners need additional schooling and a national certification to work in the NICU.
Neonatologists
Neonatologists are doctors who have specialized in pediatrics and undergone additional training to care for newborns in the intensive care unit. Their job is to diagnose and treat newborns that come into the NICU and coordinate managed care with other members of the facility. Neonatologists are the leading doctors for critically ill newborns and can work in conjunction with obstetricians, pediatricians, or family physicians for long-term care plans.
Emotional Support Staff
Entering the NICU can be an emotional experience for parents, and many hospitals often have social workers, chaplains, or other staff available to provide emotional support and counseling. If you need additional help processing your situation, ask your doctor or neonatologist for recommendations.
What to Expect if Your Baby is in the NICU
Seeing your newborn in the NICU can be a heart-wrenching experience, but the environment is meant to help your baby heal and thrive out of the womb. When visiting, you should expect to see a lot of machines, tubes, and even incubators. Although it can be alarming, all the equipment is in place to help. Some of the biggest things to prepare yourself for include the following:
Sterilizing Stations
Before entering the NICU, you must follow strict hand hygiene procedures to help prevent the spread of germs. This may include washing your hands with soap and water or using an alcohol-based hand sanitizer. Depending on the hospital's policies and the condition of your baby, you may also have to wear protective gear such as a gown, gloves, and a mask.
Controlled Environment
NICUs are typically kept at a controlled temperature and humidity level to protect the health of the infants. There may also be restricted access to the unit, and you may have to buzz in and out. The lights will be dimmed, and sound is kept to a minimum. You may also find that visitation time is limited for most family members. New parents are usually able to visit any time they’d like, but siblings, grandparents, and aunts or uncles will likely need to wait until they’re stronger.
Medical Devices
A NICU is filled with several types of medical devices, which can be a little intimidating for new parents. You should expect to see a lot of monitors, infant warmers, incubators, feeding tubes, IVs and lines, ventilators, oxygen hoods, and devices to administer phototherapy. If you have questions about any of these devices, talk to your baby’s doctor. Once you understand what they do, they can be a little less scary.
Lower Stimulation
You may notice that your newborn’s eyes are covered in the NICU. This is because a premature baby’s pupils can’t yet adjust to the changing light. Keeping them covered helps protect their eye health while allowing for the rest of the structure to develop on its own. Once they’re a bit older and have developed eye control, the coverings will be removed.
Longer Stays
You may also need to leave your baby in the hospital for some time after you’ve been discharged. This can be really stressful for many parents, but it’s important to remember that in doing so, you’re giving them the best opportunity to get better. Some NICUs have separate rooms that parents can stay in, but not all do. If you don’t live close to the hospital, ask your doctor about recommendations for hotels or nearby stays.
A Lot of Questions
Finally, after delivery, you may find friends or family reaching out to see how you and your newborn are. This can be difficult when your baby is in the NICU, but you shouldn’t feel like you have to tell everyone all of the details of what’s going on. How much you decide to talk about your baby’s condition is entirely up to you and what you’re comfortable with. You can respond with as little or as much information as you want, but you may feel better signing out of social media and turning your phone to do not disturb until you know more.
If you have a high risk pregnancy, or you’re currently pregnant after a premature birth, it’s important to work with your doctor to monitor your baby’s development and keep an eye out for potential complications. This includes women with geriatric pregnancies and women who are having multiples. Oftentimes, all this requires is seeing your doctor more often for monitoring, but you may also be put on bed rest during your third trimester. Always follow your doctor’s treatment plans and don’t hesitate to ask any questions.
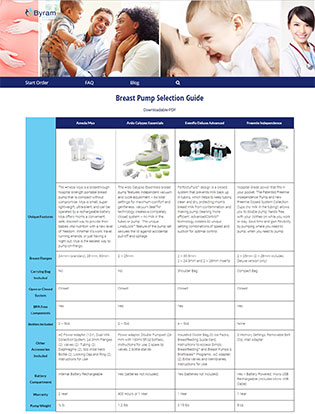
To help prepare you for parenthood, don’t forget to order an free breast pump through insurance from Byram Healthcare. Thanks to the Affordable Care Act, all new and expecting mothers are eligible to receive one at zero out of pocket costs. To learn more about your options and get started with the ordering process, check out our breast pump product selection guide today.